Prescription Drugs
-
2025 coverage cost comparison
2025
PRESCRIPTION
DRUG COMPARISONCharter Select Earn $35,00 or less Charter
BasicNexus
BasicChoice
HDHPCharter
PlusNexus
PlusChoice Annual pharmacy deductible $50 per person $100 per person $100 per person Integrated with medical $100 per person $100 per person $100 per person Prescription drugs (30-day retail)5
Tier 1 Generally Genetic $20 $20 20% 20% $20 $20 $20 Tier 2 Generally preferferd brand $60 $75 $75 20% $75 $75 $75 Tier 3 Generally Non-preferferd brand generic $100 25%
(min. $100 copay/max. $250 copay)25%
(min. $100 copay/max. $250 copay)20% 25%
(min. $100 copay/max. $250 copay)25%
(min. $100 copay/max. $250 copay)25%
(min. $100 copay/max. $250 copay)Specialty Drugs $150 25%
(min. $100 copay/max. $250 copay)25%
(min. $100 copay/max. $250 copay)20% 25%
(min. $100 copay/max. $250 copay)25%
(min. $100 copay/max. $250 copay)25%
(min. $100 copay/max. $250 copay)Prescription drugs (90-day or retail)5 Tier 1 Generally Genetic $50 $50 $50 20% $50 $50 $50 Tier 2 Generally Genetic $150 $187.50 $187.50 20% $187.50 $187.50 $187.50 Tier 3 Generally Non-preferred brand generic $250 25%
(min. $250 copay/max. $500 copay)25%
(min. $250 copay/max. $500 copay)20% 25%
(min. $250 copay/max. $500 copay)25%
(min. $250 copay/max. $500 copay)25%
(min. $250 copay/max. $500 copay)1 - Charter PCP and specialist copays do not count towards the annual deductible; but, do apply towards the annual out-of-pocket maximum.
2 - Free if you are enrolled in an HISD medical plan (not available to Choice HDHP members).
3 - Pre-certification may be required.
4 - Services are tiered under Nexus Basic and Nexus Plus.
5 - Separate pharmacy copay applies after separate pharmacy deductible has been met (except Choice HDHP). -
2024 coverage cost comparison
For additional information, view The 2024 Benefits Guide.
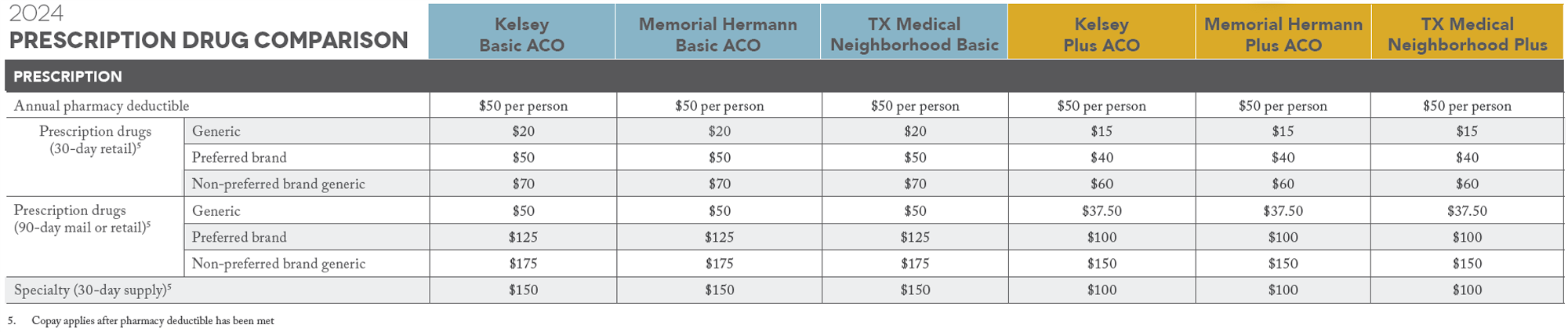
View larger 2024 Prescription Drug Comparison Chart

