Cancer and Specified Diseases
-
Supplemental coverage for major diseases
This plan includes a wellness benefit per calendar year for screening tests and provides a cash benefit for covered procedures and other care related to the diagnosis and treatment of cancer and other specified diseases. This plan pays you in addition to any other coverage you may have.You don’t need to show evidence of good health to enroll in either option.- This plan pays benefits directly to you for covered expenses resulting from the diagnosis and treatment of cancer and other specified diseases.
- 12-month pre-existing-conditions exclusion and actively-at-work provisions apply.
- You must be under age 70 to enroll.
- The cancer and specified diseases plan offers low or high coverage options.
- You can purchase group coverage to supplement your other medical coverage and help with out-of-pocket costs while being treated for cancer or one of many other specified diseases.
- This plan pays benefits directly to you for covered expenses resulting from the diagnosis and treatment of cancer and other specified diseases.
- It pays a percentage of covered expenses up to a maximum dollar limit whether you have other insurance or not.
- Some options include a wellness benefit for annual cancer screening, medications, surgeries and related hospital stays.
- This plan also covers non-medical expenses, including travel, wigs and prosthetics.
- Aflac Group administers the plan.
- No evidence of insurability is required.
For a list of plan features, see your Cancer Low or High plan certificate.
Who can enroll
You must be under age 70 and not currently diagnosed with cancer or one of the specified diseases. You cannot have been treated for internal cancer or a specified disease in the last five years and have never tested HIV-positive.
This coverage requires no evidence of insurability (EOI) for either option.
Four coverage levels
Choose between low or high coverage levels, then decide if you want to include an intensive care option. Compare details below.
With the intensive care unit rider, you receive $600 per day for every day that you or any covered person is confined in a hospital intensive care unit (ICU). This benefit is limited to 30 days per period of confinement.
You can purchase coverage for:- Employee only
- Employee + spouse
- Employee + child
- Employee + family
Pre-existing conditions
New or increased disability coverage is subject to a 3/12 pre-existing condition exclusion. If you have a condition that was treated or medically advised in the three months before your coverage effective date, you are not covered for that condition for the first 12 months.
Actively-at-work provision
If you’re not actively at work when coverage is scheduled to become effective, your coverage doesn't take effect until you complete your first day at work. Paid leave and paid vacation are not considered being actively at work.
Taking coverage with you
If you leave the district, your disability plan is convertible, unless you’re a retiree. Other exclusions may apply. For more information about conversion, click here.
Claiming benefits
If you or a covered member of your family requires a cancer screening procedure or is diagnosed with cancer or any of the specified diseases covered by your plan, send them in a claim form within 60 days, or as soon as reasonably possible.
Benefits are paid to you immediately after the claim has been received and validated. All of the benefits due are paid to you unless you assign them elsewhere.
For details, including pre-existing conditions, read your Cancer and Specified Disease Policy certificate, available here.
If you would like to review more information, click English or Spanish
Helpful resources
For more information, contact Aflac Group at 800-433-3036 between 7 a.m. and 4 p.m. weekdays, excluding holidays.
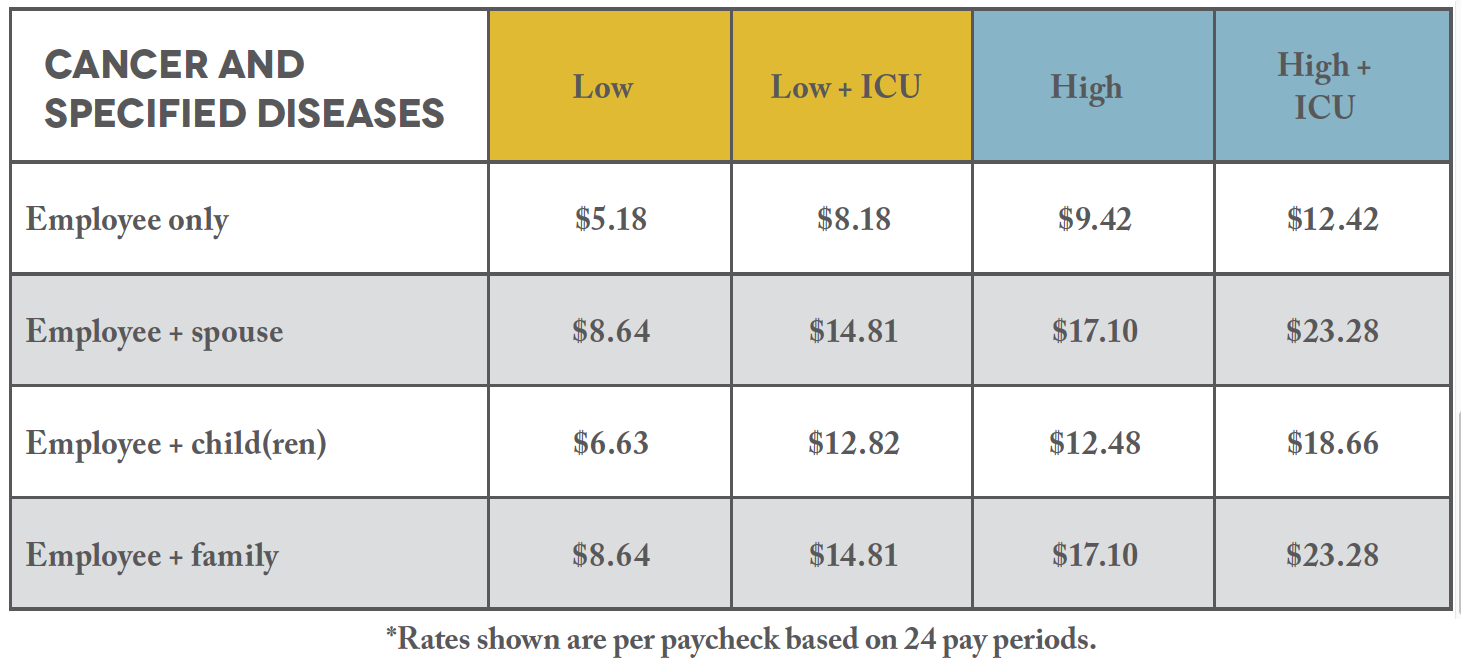
2023 COVERAGE COST
-
Cancer rates
Low option
Employee: $5.18
Employee + Spouse: $8.64
Employee + child(ren): $6.63
Employee + family: $8.64
Low option + ICU Rider
Employee: $8.18
Employee + Spouse: $14.81
Employee + child(ren): $12.82
Employee + family: $14.81
High Option
Employee: $9.42
Employee + Spouse: $17.10
Employee + child(ren): $12.48
Employee + family: $17.10
High option + ICU Rider
Employee: $12.42
Employee + Spouse: $23.28
Employee + child(ren): $18.66
Employee + family: $23.28 -
Benefit pay levels
Low option
Benefit level: $1,500
Wellness screening: $50
High option
Benefit level: $5,000
Wellness screening: $100 -
Plan features
First occurence coverage
Low option: $1,500
High option: $5,000
Wellness benefits coverage
Low option: $50/year
High option: $100/year
Hospital confinement coverage
First 30 continuous days Low option: $200/year
High option: $100/year
$200/year
Low option: $400/year coverage
High option: $600/year coverage
Surgery - inpatient/outpatient coverage
Low option: $95 - $3,000
High option: $100 - $5,000
Anesthesia
Low/High option: 25% of surgical benefit
Second surgical option coverage
Low option: $200/day
High option: $300/day
Radiation/chemotherapy coverage
Low option: $200/day
High option: $300/day
Anti-nausea medication
Low/High option: Up to $100/month
Experimental treatment coverage
Low option: Up to $200/day
High option: Up to $300/day
Blood, plasma and components coverage
Inpatient
Low option: Up to $50/day
High option: Up to $100/day
Outpatient
Low option: Up to $200/day
High option: Up to $250/day
National Cancer Institute evaluation/consultation
Low/High option: $500
Skin cancer coverage
Biopsy
Low/High option: $100
Excision of lesion of skin without flap/graft
Low/High option: $250
Excision of lesion with flap/graft
Low/High option: $600
Nursing services - in hospital coverage
Low option: $50
High option: $60
Transportation coverage
Automobile
Low option: $.40 per mile(up to $1,200 per rnd. trip)
High option: $.50 per mile(up to $1,200 per rnd. trip)
Commercial travel
Low option: $1,200
High option: $1,500
Bone marrow transplant coverage
Max in-hospital
Low/High option: $10,000
Max outpatient
Low/High option: $5,000
Bone marrow donor
Low/High option: $1,000
Stem cell transplant
High option: Incurred charges up to $2,500
Ambulance
Low/High option: Incurred charges
Prosthesis/artificial limb coverage
Surgically implanted
Low option: $2,500
High option: $3,000
Non-surgical
Low/High option: $200 coverage
Extended care facility
Low/High option: $100/day coverage
Home healthcare
Low/High option: Up to $50/day, 30 visits/year
Hospice care coverage
First 60 continuous days Low/High option: $100/day
61st day and thereafter
Low/High option: $50/day
Lifetime max per insured
Low/High option: $12,000
-
2022 Coverage Cost Comparison
Waiver of premium
Will waive premiums after 90 days of continuous disability due to cancer or covered specified disease
Specified diseases benefit
Specified diseases benefit* All of the above benefits that are available for the treatment of cancer are also available for the treatment of covered specified diseases.
Optional ICU rider
Low/High option: $600/day, up to 30 days
Covered specified diseases
Addison’s Disease
Amyotrophic Lateral Sclerosis
Cerebral Palsy
Cystic Fibrosis
Diphtheria
Encephalitis
Huntington's Chorea
Legionnaire's Disease
Malaria
Meningitis (bacterial)
Multiple Sclerosis
Muscular Dystrophy
Myasthenia Gravis
Necrotizing Fasciitis
Osteomyelitis
Poliomyelitis
Rabies
Scleroderma
Sickle Cell Anemia
Systemic Lupus
Tetanus
Tuberculosis
For a complete listing of covered specified diseases, see the plan certificates.